
23,24 In these cases ECG patterns are often atypical.

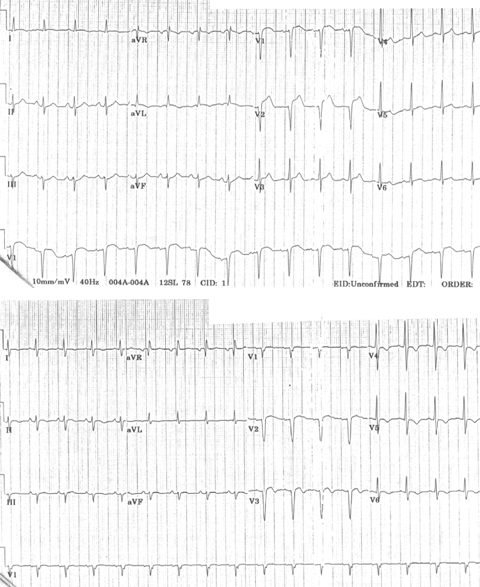
Flutter rate may be slowed by the AAD to ≤200/min, facilitating 1:1 atrioventricular (AV) conduction that due to the effect of the ADD results in aberrant intraventricular conduction and a wide QRS complex tachycardia (see Figure 4).ĬTI-dependent MRT is also frequent in patients with previous surgical atriotomies or atrial baffle procedures, or after LA ablation for the treatment of AF. One frequent presentation of flutter is in patients treated with class IC AADs for AF. Reverse typical flutter (see Figure 3) usually shows rounded or bimodal positive deflections in inferior leads II, III and aVF, and a very characteristic bimodal negative wave in the shape of a W is seen in lead V1. Atrial deflections in V1 can be positive, biphasic or negative. Typical (counter clockwise) flutter is associated with the ‘common’ flutter pattern 20,21 (see Figure 2): a regular continuous undulation with dominant negative deflections in inferior leads II, III and aVF, often described also as a ‘saw tooth pattern’, and flat atrial deflections in leads I and aVL. 19 This reverse typical flutter is much less common clinically than the counter clockwise form, but the clinical manifestations are indistinguishable. superoinferior in the septal wall and inferosuperior in the anterolateral wall – with the same zones of block in the posterior RA and obligatory passage through the CTI (see Figure 3). 16–18 In either case, the CTI remains an obligatory passage for activation in the inferior RA.Įither spontaneously or after programmed stimulation, re-entry may occur in the opposite (clockwise) direction – i.e. An area of transverse conduction block in the posterior RA related to anisotropic conduction at the terminal crest 11–14 and other structures15 forces activation toward the high RA so that the upper turning point can be at the RA roof or high in the posterior RA, depending of the size of the area of block. 10 Activation courses superoinferiorly in the anterior and lateral RA and inferosuperiorly in the septal RA, with a critical inferior turning point between the tricuspid ring and inferior vena cava (IVC) known as the cavotricuspid isthmus (CTI) (see Figure 2). The mechanism is a large re-entrant circuit contained in the right atrium (RA) with passive activation of the left atrium (LA). Typical flutter is the type of MRT most frequently found in the clinical setting.
Modern electrophysiology (EP) has confirmed the re-entrant mechanism of typical flutter, and has opened wide the spectrum of mechanisms of macro-re-entrant tachycardias (MRTs), prompting a new, more open view of clinical ECG-based classification (see Figure 1A and 1B). 8 This was not a significant consideration when digitalis and very few antiarrhythmic drugs (AADs) were the only therapeutic armamentarium, but determining the mechanism involved in flutter has become crucial for the design and application of catheter and surgical ablation techniques. 6,7 Later human studies left the door open for a focal mechanism. Early studies suggested that flutter had a re-entrant mechanism 3–5 but others attributed flutter to focal discharge.

Slower tachycardias displaying discrete P waves, separated by isoelectric baselines, were called ‘atrial tachycardia’. 1,2 On the ECG, flutter was a regular continuous undulation between QRS complexes at a cycle length (CL) of ≤250 ms (≥240 bpm). The term ‘flutter’ was coined to designate the visual and tactile rapid, regular atrial contraction induced by faradic stimulation in animal hearts, in contrast with irregular, vermiform contraction in atrial fibrillation (AF). In patients subjected to cardiac surgery or catheter ablation for the treatment of atrial fibrillation or showing atypical ECG patterns, macro-re-entrant and focal tachycardia mechanisms can be very complex and electrophysiological studies are necessary to guide ablation treatment in poorly tolerated cases. Secondary prevention, based on the treatment of associated atrial fibrillation risk factors, is emerging as a therapeutic option. In patients without a history of heart disease, cardiac surgery or catheter ablation, typical flutter ECG remains predictive of a right atrial re-entry circuit dependent on the inferior vena cava–tricuspid isthmus that can be very effectively treated by ablation, although late incidence of atrial fibrillation remains a problem. Electrophysiological studies have defined multiple mechanisms of tachycardia, both re-entrant and focal, with varying ECG morphologies and rates, authenticated by the results of catheter ablation of the focal triggers or critical isthmuses of re-entry circuits. Clinical electrophysiology has made the traditional classification of rapid atrial rhythms into flutter and tachycardia of little clinical use.


 0 kommentar(er)
0 kommentar(er)
